Talk with a ChartSpan Representative Today!
Our team is ready to help you improve patient care and outcomes.
Blog
G0511: What RHCs and FQHCs Can Do When The Code Disappears
CMS introduced Code G0511 in the Physician Fee Schedule Final Rule for 2018. In the years since, this bundled care management code has become a vital source of Medicare reimbursements for many Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs).
But the Physician Fee Schedule Final Rule for 2025 brought a major shift, as CMS officially retired code G0511. Beginning July 1, 2025, FQHCs and RHCs must bill each care management service separately, using the same codes that other healthcare practices do.
This change is stressful for many RHCs and FQHCs, who rely on G0511 reimbursements to continue providing care to their vulnerable patient populations. Fortunately, you have multiple options for how to protect your practice’s reimbursements while continuing to offer care management to your patients.
The first option is to bill for individual care management services, such as Chronic Care Management, while incorporating the add-on codes that traditional facilities already have access to. The second is to switch to a new, bundled care management program, Advanced Primary Care Management. We’ll break down both options and how you can decide which is right for your practice.
The End of G0511
From January 2018 to June 2025, RHCs and FQHCs were able to bill the code G0511 for multiple forms of care management. Initially, G0511 was used for Chronic Care Management (CCM) and Behavioral Health Integration (BHI).
Later, more codes were added for Transitional Care Management (TCM), Remote Physiological Monitoring (RPM), Remote Therapeutic Monitoring (RTM), Principal Care Management (PCM), Principal Illness Navigation and Principal Illness Navigation - Peer Support (PIN and PIN-PS), and Community Health Integration (CHI).
RHCs and FQHCs could bill G0511 for any of these services, as well as for combinations of these services. One RHC might bill G0511 for Chronic Care Management, while another billed it for CCM and for RPM.
FQHCs and RHCs benefited from higher reimbursements than traditional practices for these services under G0511. In 2025, a traditional practice would receive an average of $60 per patient, per month for CCM under code 99490. Under code G0511 before its sunset, an RHC or FQHC could receive $72 per patient, per month.
However, since G0511 bundled so many different types of services together, FQHCs and RHCs were not paid separately for separate programs. Because of this limitation, in the CY 2024 Final Rule, CMS allowed RHCs and FQHCs to bill G0511 more than once in a month as long as all requirements were met for each service and there was no overlap in resource time.
This policy changed in 2025. CMS stated in the CY 2025 Final Rule that they wished to identify the individual services provided. They therefore required RHCs and FQHCs to begin billing the individual codes that make up G0511 beginning on July 1, 2025. RHCs and FQHCs that already had billing infrastructure in place could switch to individual codes as early as January 1, 2025, but CMS stated that the entire facility must switch from G0511 to individual codes at the same time.
Increasing Reimbursements with Add-on Codes
RHCs and FQHCs that offer a wide array of care management services may be able to bill enough individual codes to not lose revenue* after the end of G0511. For most practices, however, the loss of G0511 will result in a noticeable decline in reimbursements.
If your practice currently bills for Chronic Care Management, for example, your reimbursements could decline by as much as 20% per patient, per month. CMS acknowledged this possibility and suggested that some of this decline could be offset by add-on codes.
For Chronic Care Management, this would mean adding code 99439 to code 99490. 99439 adds $46 for every additional 20 minutes of care a patient requires, up to 60 minutes of care. If a patient needed 45 minutes of care in a month, the practice could bill 99490, then bill 99439 once for the extra 20 minutes. If the patient went up to 60 minutes, the practice could bill 99439 twice.
However, many patients won’t require 20 to 40 additional minutes of CCM care, so the add-on code can only be used for a small percentage of the population. Other add-on codes, such as 99494 for BHI or 99427 for PCM, present the same challenge. They can help offset reductions in reimbursements, but only when patients require additional time spent.
If you don’t want to launch a new care management program, utilizing add-on codes with individual care management codes is the most straightforward way to compensate for reduced reimbursements. But if you’re concerned your RHC or FQHC doesn’t have a large enough population of patients who require extra minutes of care, you may want to consider Advanced Primary Care Management, a program that isn’t time-based.
The Option of Advanced Primary Care Management
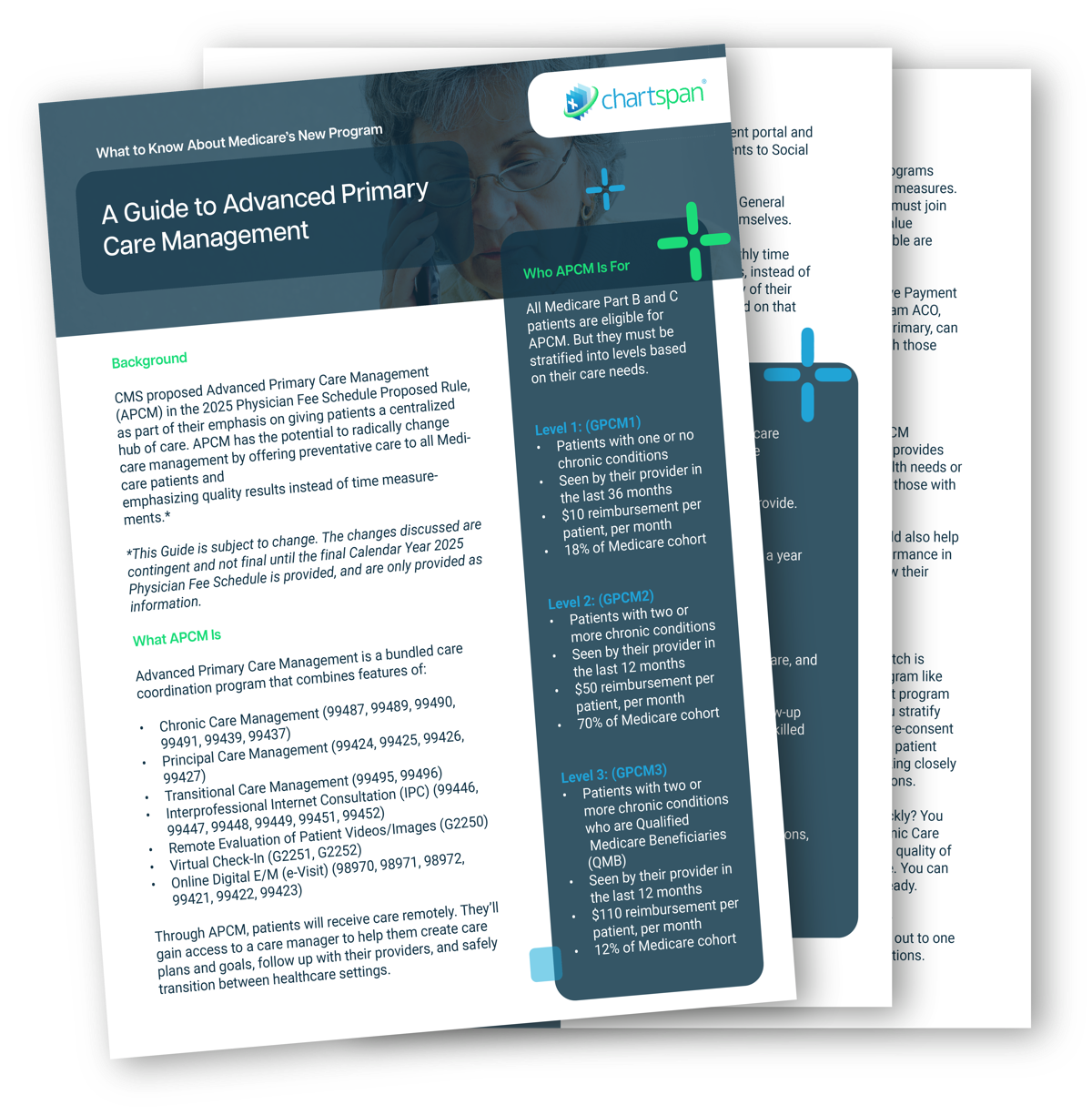
The same year that CMS retired code G0511, they introduced a new care management program, Advanced Primary Care Management. Advanced Primary Care Management combines elements of Chronic Care Management, Transitional Care Management, and Primary Care Management. However, unlike those programs, it is not time-based.
Advanced Primary Care Management includes an extensive list of service offerings. Practices can bill for APCM any month the patient is enrolled and has access to the service capabilities, even if the patient doesn’t use them that month. This allows practices to adjust the care they provide based on patients’ needs.
The requirements for offering APCM services include:
- Patient consent
- An initiating visit if you have not seen the patient in the past three years
- 24/7 access and continuity of care
- Comprehensive care management, including needs assessments, directions to preventive services, and medication reconciliation and management
- Electronic, patient-centered comprehensive care plan
- Coordination of care transitions after an Emergency Department visit or hospital discharge
- Coordination of practitioner, home-, and community-based care
- Enhanced communication opportunities (ex. online portals, email, texting)
- Patient population-level management, including identifying gaps in care and risk stratification
- Measure and report performance through the Value in Primary Care MIPS Value Pathway (if MIPS-eligible) or an ACO, such as ACO Reach
Many of these features, like 24/7 access to care, care managers and an electronic care plan, are part of Chronic Care Management and Principal Care Management. However, APCM also adds other features that are valuable to patients, like coordination of care transitions, population-level identification of gaps in care, and coordination of home- and community-based care in collaboration with the practice.
APCM is also different from other care management programs because it is available to all Medicare patients, even those with no chronic conditions. However, reimbursements are higher for offering APCM to Qualified Medicare Beneficiaries, a patient population FQHCs and RHCs often serve.
Who Qualifies for APCM?
Advanced Primary Care Management empowers RHCs and FQHCs to offer care management to all of their Medicare patients but varies reimbursements based on patient acuity. Average national reimbursements in 2025 were:
Level 1 (patients with one or no chronic conditions): $15 per patient, per month
Level 2 (patients with two or more chronic conditions): $50 pppm
Level 3: (Qualified Medicare Beneficiaries with two or more chronic conditions): $110 pppm
22% of rural patients have 2-3 chronic conditions, compared to 18.9% of patients in metropolitan areas. RHCs are therefore likely to have higher rates of Level 2 patients. Both RHCs and FQHCs also serve large numbers of low-income patients, leading to potentially higher rates of Qualified Medicare Beneficiaries.
Qualified Medicare Beneficiaries have no cost-sharing for Advanced Primary Care Management and can greatly benefit from its services, like a dedicated care manager who can recommend Social Determinant of Health resources. RHCs and FQHCs can also benefit from higher monthly reimbursements for Level 3 patients, which can help compensate for the loss of G0511 and ensure you can continue offering services to your patients.
Choosing a Path Forward
When G0511 disappears, RHCs and FQHCs will face a dilemma. You can:
- Bill only for standard care management codes
- Bill for standard care management codes and their add-on codes
- Switch to Advanced Primary Care Management
While billing for standard care management codes will be the easiest transition, it will lead to lower reimbursements. You can offset these lower reimbursements by using add-on codes, but those will only be available for patients who require extra minutes of care.
Advanced Primary Care Management is not time-based and is available to all patients. It also has higher reimbursements for Qualified Medicare Beneficiaries, a group of patients FQHCs and RHCs often serve. However, it requires switching to a new program with new service requirements.
As a provider of Chronic Care Management and Advanced Primary Care Management, ChartSpan can help your practice transition to new billing codes or a new program when G0511 ends. To learn more about how each of these care management programs can benefit your practice, visit:
*Results may vary by provider.
Subscribe for More Insights
Get valuable resources delivered straight to your inbox.
"*" indicates required fields