
Talk with a ChartSpan Representative Today!
Our team is ready to help you improve patient care and outcomes.
Blog
How CCM Helps You Address Care Gaps in Healthcare: from Screenings to SDOH
Gaps in care dramatically impact patients’ health. When patients don’t receive recommended assessments, vaccinations or screenings, they can fall ill from preventable diseases, see their chronic conditions worsen, and experience lower quality of life.
Practices that effectively address care gaps in healthcare see substantial benefits, such as financial incentives from CMS, help fulfilling regulatory compliance and reporting requirements, and success meeting performance expectations from health plan partners, ensuring strong contractual relationships.
However, healthcare practices who don’t perform well when addressing gaps in care receive lower scores in quality programs and lower reimbursements for their value-based care programs. Though your practice might be keenly aware of the need to address gaps in care, you might also lack the staff or hours to do so.
Preventive care programs, like Chronic Care Management, can help identify and address care gaps before they lead to worse health outcomes for patients. CCM and other care management programs can give patients greater access to preventive care while helping providers improve their quality measures.
How Chronic Care Management Assists Patients
Through Chronic Care Management, Medicare patients who have two or more chronic conditions receive preventive care every month. Once patients enroll, they’ll have monthly check-ins with a care coordinator and access to a 24/7 phone and text line.
Their care coordinator can help them:
- Create care plans and goals
- Schedule or reschedule appointments
- Refill their prescriptions
- Check their blood pressure or blood sugar
- And find community resources
Their care coordinator can also address some of the most common gaps in care among older patients, such as breast and colon cancer screenings, Hb A1C tests, or adult vaccinations.
Care Gaps in Healthcare CCM Can Address
Because CCM care coordinators call patients every month, they have more opportunities to speak with patients than practices typically do. This gives them multiple chances to address care gaps that commonly occur for Medicare patients.
Recommended screenings, tests, and vaccinations for Medicare patients might include:
Tests and Screenings
- Diabetic Eye Exams
- Hemoglobin A1C Tests
- Blood Pressure Measurement
- Depression Screening
- Cognitive Assessment
- Smoking Cessation Screening
- Breast Cancer Screening
- Colorectal Cancer Screening
- BMI Screening and Follow-up
Vaccinations
- Pneumonia Vaccination
- Herpes Zoster Vaccination
- Influenza Vaccination
- Tetanus/Diphtheria Vaccination (tDAP)
While these are some of the most common gaps in preventive care, patients may also need other screenings or immunizations based on their age, gender, and health conditions. For example, some patients may require fall risk or medication adherence screening.
How Care Coordinators Address Gaps in Care
If care coordinators notice a patient has a care gap in their record, they can ask the patient if they would like to address that gap. The care coordinator can then perform the assessment; note that the patient has already had the screening, vaccination or assessment at another location; record that the patient declined the service; or refer the patient back to the practice for in-person care.
At ChartSpan, we have a dedicated Quality Improvement team who can create documentation of care gaps and care gap performance, then share that information with practices. Together, the practice and the quality team can decide which care gaps to prioritize.
In addition to ensuring patients have the proactive assessments, tests, and screenings they need, this process helps practices improve their performance on quality measures and raise their quality scores. This is essential for practices who participate in programs like MIPS, ACOs, or AAPMs.
Quality Programs CCM Assists With
Most practices participate in programs that require them to report quality measures for their Medicare patients. Some of the quality programs ChartSpan encounters most frequently include:
- Merit-based Incentive Payment System (MIPS)
- MIPS Value Pathways (MVPs)
- Accountable Care Organizations (ACOs), including the Medicare Shared Savings Program (MSSP)
- Medicare hospital star ratings
- Advanced Alternative Payment Models (AAPMs)
Each of these programs comes with a different set of quality measures, and achieving success on these measures can impact hospitals’ and practices’ Medicare reimbursements.
To effectively improve quality scores, Chronic Care Management organizations must understand what quality programs the practice participates in. At ChartSpan, we offer a complimentary Quality Improvement team who can consult with the practice on their quality programs and which measures they need to address most urgently. ChartSpan and the practice then work together on a plan to address those care gaps.
The Results of Using CCM to Address Care Gaps in Healthcare
Through regular check-ins with patients, performing assessments, assembling medical records from multiple locations, and referring patients back to the practice, care coordinators are able to address multiple gaps in care.
In ChartSpan’s CCM program, 100% of engaged patients receive clinical assessments like:
- Condition Awareness Screening
- Activities of Daily Living Screening
If the assessment indicates that the patient needs support, their care coordinator can refer them back to their provider. Care coordinators can also help patients find local resources, like transportation, prescription delivery services, medical equipment agencies, and support groups.
The ability to quickly identify and address Social Determinants of Health needs is especially important. Access to resources like safe housing, reliable transportation, and nutritious food can have a dramatic impact on health outcomes.
Care coordinators can perform SDOH screenings during monthly calls. If a screening identifies that a patient needs support, the care coordinator can direct them to food pantries, housing agencies, utilities assistance, senior centers, and other resources in their community.
Gaps in Care and Quality Assessments
In addition to helping with clinical assessments, ChartSpan’s quality team can partner with providers to address gaps in care for specific patients.
In 2024, ChartSpan’s care coordinators identified and addressed 33,447 gaps in care. 15,849 patients reported they’d already had the relevant assessment, screening or vaccination, allowing us to update their records and inform their provider. 1,211 asked us for help completing a phone-based assessment or scheduling a screening, vaccination, or appointment.
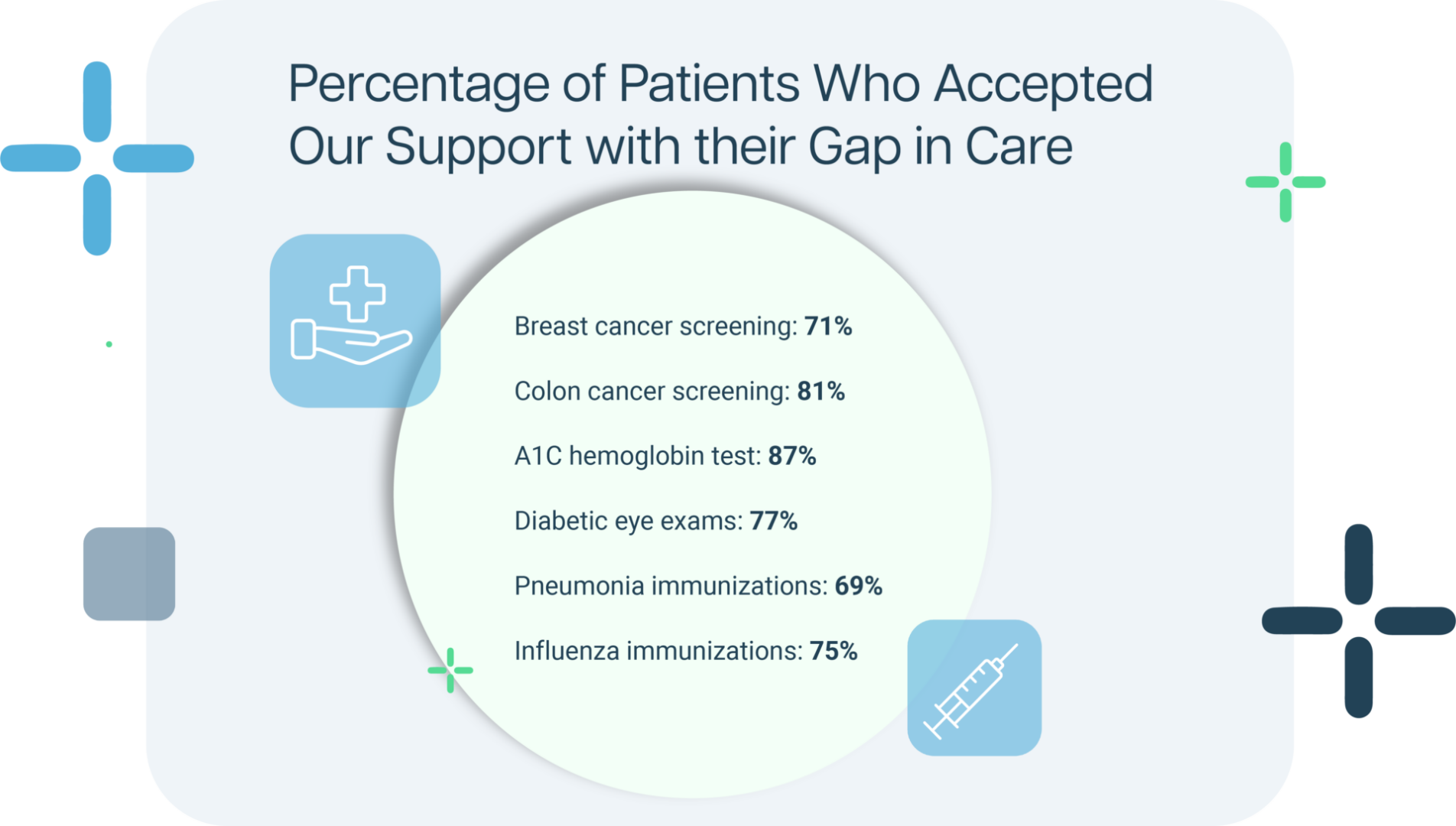
All in all, 51% of patients with a gap in care asked for our assistance in addressing it. For certain gaps in care, the percentage of patients asking for our support rose even higher.
For these patients, we were able to update their records to show the gap in care was already closed or make an appointment so their provider could close the gap in care. If a patient hasn’t received a relevant immunization, screening, or test, their care coordinator can offer education on why the assessment is important and help them with transportation and appointment scheduling. These reminders help patients receive preventive care more frequently and lower their risk of serious illness.
Why Addressing Gaps in Care Matters
By identifying and addressing gaps in care, Chronic Care Management can help patients prevent and manage illness, leading to better long-term health outcomes. At the same time, practices could see improvements in their value-based care and quality performance.
Chronic Care Management gives practices multiple opportunities to address care gaps with Medicare patients, up to twelve times a year. Care coordinators build relationships with patients while ensuring they have access to needed screenings, vaccinations, SDOH resources, and assessments.
If you’d like to learn more about CCM’s impact on patients, you can view how CCM reduces hospital readmissions and healthcare costs in ChartSpan’s claims data report.
Subscribe for More Insights
Get valuable resources delivered straight to your inbox.
"*" indicates required fields






