Talk with a ChartSpan Representative Today!
Our team is ready to help you improve patient care and outcomes.
Blog
Major Updates from the 2025 Medicare Physician Fee Schedule Final Rule
The 2025 Medicare Physician Fee Schedule Final Rule will bring significant changes to how practices are reimbursed by Medicare. In addition to a new conversion factor for all practices, the Final Rule introduces major billing changes and a brand-new service, called Advanced Primary Care Management, which will transform how practices and health systems engage in preventative care.
If your practice or health system serves Medicare patients, it’s time to prepare for the changes 2025 will bring to the Physician Fee Schedule. We’ll break down how your reimbursements will change and the new programs that will bring an unprecedented level of care to your Medicare patients.
1) Changes to the PFS Conversion Factor
In the Final Rule, the Centers for Medicare & Medicaid Services estimate that the conversion factor for 2025 will be 32.35. In 2024 the conversion factor started at 32.74, before the Consolidated Appropriations Act of March 2024 raised it to 33.29. This means that in 2025, practices could see a 2.83% decrease in their Medicare payments, leading to less revenue overall.
It’s possible Congress will once again choose to raise the conversion factor for 2025 or introduce legislation that eliminates reimbursement reductions. However, based only on the Final Rule, practices need to prepare for another drop in their conversion rates and reimbursements.
2) Elimination of G0511 for RHCs and FQHCs
Throughout 2024, Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs) were able to bill the code G0511 for multiple forms of care management: Chronic Care Management (CCM), Behavioral Health Integration (BHI), and even Remote Patient Monitoring (RPM).
G0511 reimbursement was higher than the reimbursement traditional ambulatory practices received for these services, and RHCs and FQHCs could bill G0511 multiple times in the same month. However, all care management services were grouped together under the same code.
The Final Rule states that beginning in July 2025, code G0511 will no longer be payable for RHCs and FQHCs. Instead, RHCs and FQHCs will bill each of their care management services individually, using the same codes that traditional ambulatory practices do. For example, RHCs and FQHCs would now bill 99490 for non-complex Chronic Care Management and 99439 for additional time beyond twenty minutes of Chronic Care Management.
CMS first proposed the elimination of G0511 for January 2025, but CMS delayed the implementation until July 1, 2025 to give RHCs and FQHCs time to adjust their billing systems.
RHCs and FQHCs who don’t want to bill each care management service separately can consider offering a new, optional program called Advanced Primary Care Management instead.
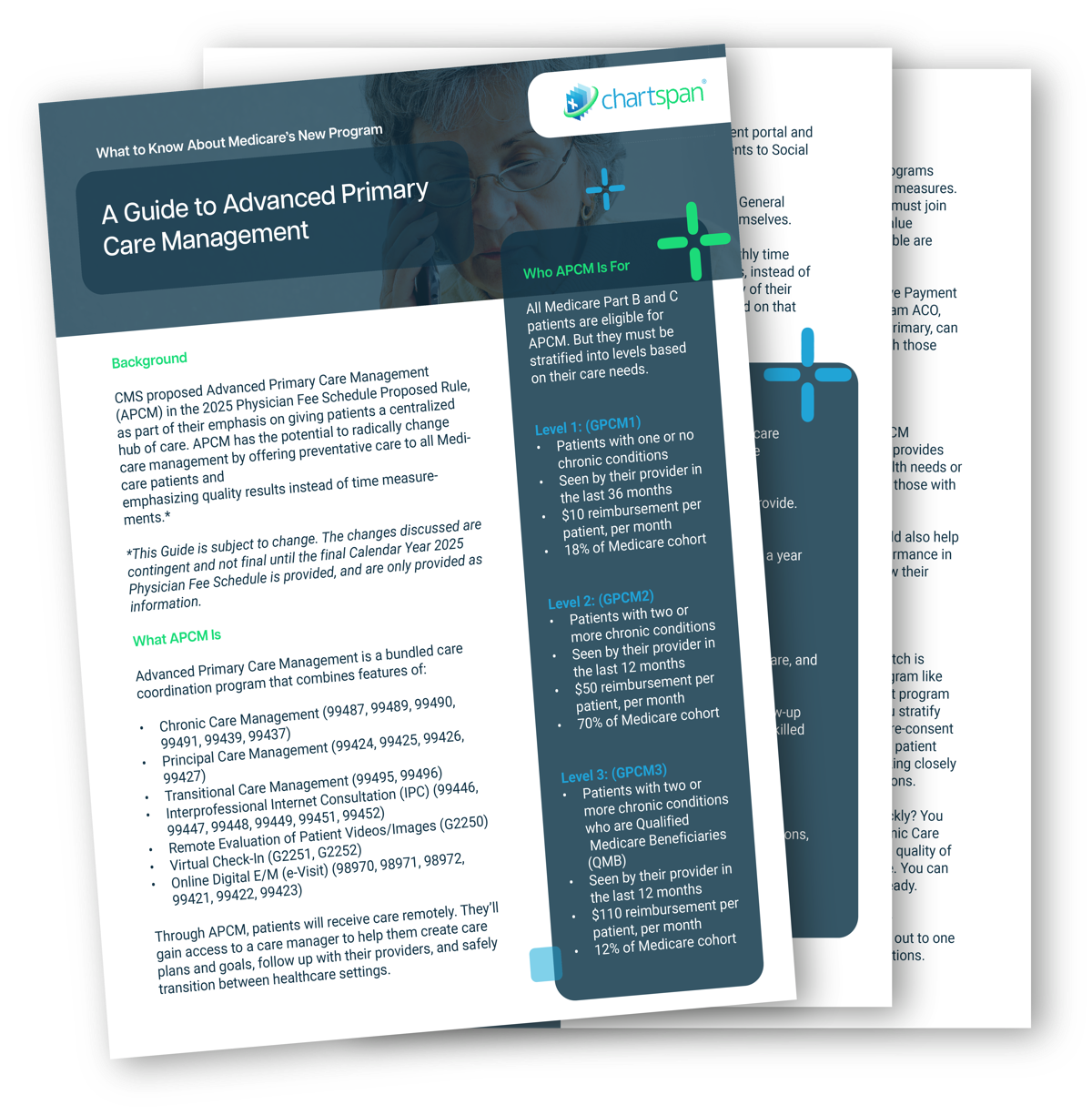
3) New Program: Advanced Primary Care Management
The Final Rule for the 2025 Medicare Physician Fee Schedule introduces a new preventative care program: Advanced Primary Care Management. Care management has long been a focus for CMS, with programs like Transitional Care Management and Chronic Care Management becoming staples for many practices.
Advanced Primary Care Management will transform preventative care by combining multiple care management and telehealth programs into a single program. The APCM program will incorporate features of:
- Chronic Care Management
- Transitional Care Management
- Principal Care Management
- Interprofessional Internet Consultation
- Remote Evaluation of Patient Videos/Images
- Virtual Check-In
- Online Digital E/M (e-Visit)
As the name implies, Advanced Primary Care Management will be available for primary care practices, including general, geriatric, family, and internal medicine practices. But CMS also proposes that some specialists who serve as a primary source of care, like cardiologists and OB-GYNs, can offer the program.
Risk-Stratification for Billing APCM
One of the biggest differentiators in Advanced Primary Care Management compared to existing care management programs is that it expands eligibility. Furthermore, patients are separated into three levels, depending on the acuity of the patient. Each level has its own corresponding HCPCS codes, requirements, and reimbursements levels.
Level 1: Requirements for G0556
Medicare patients with one or fewer chronic conditions
$15 per patient, per month reimbursement
Level 2: Requirements for G0557
Medicare patients with two or more chronic conditions
$50 per patient, per month reimbursement
Level 3: Requirements for G0558
Patients with two or more chronic conditions who are Qualified Medicare Beneficiaries (QMB)
$110 per patient, per month reimbursement
Removal of Time Thresholds
In addition to being offered to all Medicare patients, Advanced Primary Care Management differs from other care management programs because it’s not time-based. CMS has removed the minimum clinical time worked requirements for monthly care, such as the 20 minutes required under non-complex Chronic Care Management (99490). Clinical staff are expected to spend as much time on care as the patient requires.
Clinical staff members can also adjust care based on factors like whether the patient has recently been admitted to the hospital, whether they’re ill or coping with complications from their chronic condition, and whether they’ve been taking their medications regularly. Depending on the patients’ needs, the clinical staff can help with care plans and goals, provide directions to local community resources, or assist with setting appointments and scheduling medication refills.
Advanced Primary Care Management can take place under general supervision. This means clinical staff can perform the services, while the patient’s provider supervises the overall process. Practices are allowed to partner with care management organizations to offer APCM without overwhelming their workforce.
APCM Service Elements
Since APCM combines the service elements of several care management programs, service providers are expected to expand their care program to meet additional needs.
- Consent
While all Medicare patients are eligible for Advanced Primary Care Management, they must consent to receive the services. Patients also can’t be enrolled in Advanced Primary Care Management at the same time as other care management services, like Chronic Care Management, Principal Care Management, or Transitional Care Management.
Clinical staff must ask patients if they would like to enroll and inform them that they can only be enrolled under one provider and can unenroll at any time. Patients must also agree to cost-sharing, unless they are a Qualified Medicare Beneficiary. (QMBs are exempt from copays and deductibles.) Consent must be recorded in the patient’s record.
- Initiating Visit for New Patients
New patients must have an initiating visit. An initiating visit is not required if the patient has been seen by the provider or another provider at the same practice within the past three years.
- 24/7 Access to Care and Care Continuity
A member of the care team with access to the patients’ health records must be available to patients 24 hours a day. There also must be a way to contact health care professionals in the practice after hours to discuss urgent needs. The patient should be able to visit the same member of the care team for successive routine appointments, and the practice should supplement traditional office visits with accessible offerings like expanded office hours or home visits.
- Comprehensive Care Management
Comprehensive care management should include systematic assessments of patients’ physical and psychosocial needs, systems to ensure patients receive preventative care, and medication reconciliation, management, and assistance with self-management.
- Patient-Centered Comprehensive Care Plan
Care coordinators must work with patients to create, implement, revise and maintain an electronic care plan. This document needs to be accessible to everyone involved in a patient’s care, from the provider to the care team, the patient, and the patient’s caregivers.
- Management of Care Transitions
Care managers must oversee transitions from one healthcare setting to another, whether patients were referred to a specialist, went home after visiting the emergency department visit, or were released from a hospital or a skilled nursing facility. The care manager must exchange electronic information with other providers involved in the patient’s care and must follow up with the patient within seven days of their discharge.
- Practitioner, Home–, and Community–Based Care Coordination
The care manager must help patients find and receive assistance from practitioners, home– and community-based services, social service agencies, hospitals, and skilled nursing facilities, as needed. The care manager must also document the patients’ psychosocial strengths, needs, goals, and desired outcomes, while noting their cultural and linguistic preferences.
- Enhanced Communication Opportunities
The patient must be able to communicate with their care team and their provider through multiple methods, including secure messaging, email, Internet, patient portal, or phone. Providers should also be able to review and evaluate pre-recorded images or videos from patients. Practices must offer digital communication options that can provide a clinical decision, like virtual check-ins or e-visits.
- Patient Population-Level Management
Practices must analyze patient population data to identify gaps in care and offer interventions. They must also have the ability to risk-stratify their patients according to the three levels of APCM.
- Performance Measurement
One of the most significant differences between Advanced Primary Care Management and programs like CCM or PCM is that APCM is outcomes-based. To prove that they are providing quality, cost-effective care, practitioners who are MIPS-eligible need to register for the Value in Primary Care MIPS Value Pathway. Providers who are not MIPS-eligible, such as RHCs and FQHCs, can still participate in the program.
APCM is also open to providers who are enrolled in the Medicare Shared Savings Program, ACO Reach, Making Care Primary, or Primary Care First programs. All of these programs are used to track patient outcomes and evaluate whether APCM has been effective.
Navigating the Changes to the Medicare Physician Fee Schedule
The Medicare Physician Fee Schedule will undergo major changes in 2025. Reimbursement rates for services will drop, and FQHCs and RHCs will no longer be able to bill G0511 starting in July 2025.
However, FQHCs and RHCs will gain the ability to bill care management services separately. All practices will also have the option to embrace a new care management program, Advanced Primary Care Management, which ensures Medicare patients have 24-hour access to care.
If you’d like to learn more about Advanced Primary Care Management and other provisions of the PFS, reach out with your questions at https://www.chartspan.com/contact-us/. Checking out this blog in November 2024? Join us for our upcoming educational webinar to learn more about changes to the Physician Fee Schedule.
Sources
Centers for Medicare & Medicaid Services. (2024, November 1). 2025 Medicare Physician Fee Schedule Final Rule. Federal Register.
https://public-inspection.federalregister.gov/2024-25382.pdf
Subscribe for More Insights
Get valuable resources delivered straight to your inbox.
"*" indicates required fields