Talk with a ChartSpan Representative Today!
Our team is ready to help you improve patient care and outcomes.
Blog
What is a QMB/Qualified Medicare Beneficiary?
The Qualified Medicare Beneficiary program is one of four Medicare Savings Programs sponsored by Medicaid. Although Medicare ensures that qualifying patients have healthcare coverage, patients may still have to pay deductibles, copays or coinsurance, which can be a challenge for lower-income patients. The QMB program and other Medicare savings programs assist with these costs.
Hospitals, health systems and practices need to understand the QMB program because it directly impacts billing. Providers and suppliers, such as pharmacies, are prohibited by law from billing QMB patients for deductibles, coinsurance or copays for Medicare Part A and B services. Therefore, it’s critical that you understand what a QMB is, which patients qualify for the program, and which preventative care programs are impacted by QMB status.
What is a Qualified Medicare Beneficiary?
Qualified Medicare Beneficiaries are dual-eligible Medicare beneficiaries with income and resources at or below the federal poverty line, who applied and were accepted into the QMB program. Once they’re accepted, the QMB program covers their Medicare Part A premiums, Part B premiums, deductibles, coinsurance and copays. About 8 million people, or 1 in 8 Medicare beneficiaries, were in the QMB group in 2023.
Some QMB patients do not have additional Medicaid coverage. These patients are known as “QMB Only.” Other QMB patients have full Medicaid coverage and are known as “QMB Plus.” However, whether a patient is QMB Only or QMB Plus, they will have no cost-sharing for covered Medicare parts A and B services.
How do patients become QMBs?
Patients must apply for Medicare savings programs through their state. The state will then determine whether they meet the requirements for the Qualified Medicare Beneficiary group.
Federal guidelines offer the following income limits for QMBs, as of 2025:
Individual
- Monthly income limit: $1,325
- Resource limit: $9,660
Married Couple
- Monthly income limit: $1,783
- Resource limit: $14,470
While most states use these guidelines, some may set higher income limits or waive the asset guidelines. Therefore, patients may qualify as QMBs even if they fall outside of these limits.
How do providers and suppliers find out which patients are Qualified Medicare Beneficiaries?
All original Medicare and Medicare Advantage providers and suppliers cannot charge Qualified Medicare Beneficiaries for Medicare cost-sharing for covered Part A and Part B services. If a QMB patient accidentally receives a bill, the practice must recall the bill and refund any costs the patient has paid.
Therefore, it’s important to have methods for determining which patients are QMBs. CMS offers several ways for providers and suppliers to make this determination:
- HIPAA Eligibility Transaction System (HETS)
The HIPAA Eligibility Transaction System, or HETS, contains Medicare eligibility data for Medicare providers, suppliers, and authorized billing agents, including third-party vendors.
Practices or health systems can access HETS to verify a patient’s QMB status. They can also ask third-party vendors they work with if their products reflect QMB information from HETS. To better perform our role as a care management vendor, ChartSpan has access to QMB information from the HETS database.
- Medicare Provider Remittance Advice
Original Medicare providers and suppliers can identify patients’ QMB status by checking the Medicare Provider Remittance Advice, which is provided by their Medicare claims processing contractor.
- Medicare Advantage Plans
Medicare Advantage providers and suppliers can contact the Medicare Advantage program directly to learn the QMB status of plan members.
- State Medicaid Eligibility Systems
Providers and suppliers can also verify a patient’s QMB status through their state’s online Medicaid eligibility system. Some states provide additional documentation, including Medicaid identification cards, Medicare Summary Notices, or other documents, that show the patient is enrolled in the QMB program.
- Patient Documentation
Sometimes patients will present evidence of their QMB status at the practice or health system. They may present some combination of their original Medicare, Medicaid or QMB cards, or one of their Medicare Summary Notices.
While practices or health systems have multiple options for verifying patients’ QMB status, you may find it easiest to work with a vendor who has HETS access built into their software, so you don’t have to engage in additional steps.
Which Medicare programs are impacted by Qualified Medicare Beneficiaries?
All Medicare Parts A and B services are impacted by QMB status, since QMB patients do not pay for Medicare deductibles, copays or coinsurance. However, QMB status has received increased attention in 2025 due to the introduction of Medicare’s new care management program, Advanced Primary Care Management.
Advanced Primary Care Management and Qualified Medicare Beneficiaries
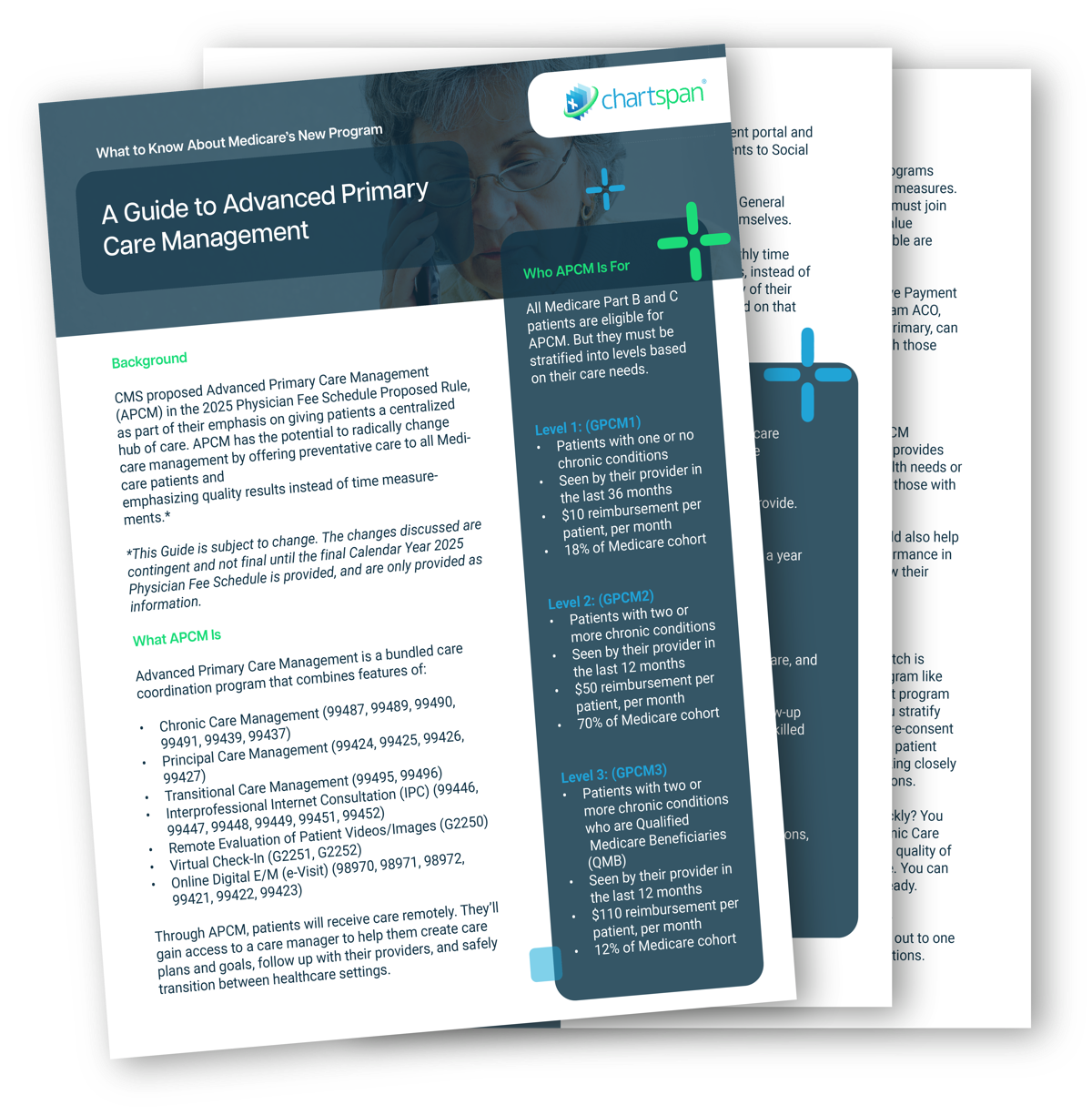
Advanced Primary Care Management offers preventative care to all Medicare patients. But it also separates patients into levels to help care managers adapt their care to the acuity of the patients’ health needs. The third level of APCM is reserved for Qualified Medicare Beneficiaries only.
Level 1 of Advanced Primary Care Management is for patients with one or no chronic conditions, and reimburses providers at the lowest rate. The national reimbursement average is only $15 per patient, per month.
Level 2 is for patients with two or more chronic conditions, and reimburses at a national average of $50 per patient, per month.
Level 3 is reserved for Qualified Medicare Beneficiaries who have two or more chronic conditions. It reimburses at the highest rate, with a national average of $110 per patient, per month.
Because this third level of reimbursement is so high, and because Qualified Medicare Beneficiaries often benefit from preventative care and Social Determinant of Health resources, many providers are eager to determine how many QMB patients they have before embarking on Advanced Primary Care Management.
How to Determine QMB Eligibility Before Launching APCM
If you are launching an in-house APCM program, you’ll need a reliable way to determine which patients are Qualified Medicare Beneficiaries, such as accessing the HETS system. However, if you’re partnering with a third-party organization, they can often make eligibility determinations for you.
If you choose to partner with ChartSpan, we have the ability to access the HETS database and determine which of your Medicare patients are Qualified Medicare Beneficiaries. We then present you with the list so you’re informed and can decide which patients you’d like us to reach out to about enrolling in Advanced Primary Care Management.
APCM Services for QMB Patients
QMB patients who choose to enroll in APCM will have no copay, just as they have no copay for other Medicare Part A and B services. They will also receive resources that are vital for many QMBs, such as Social Determinant of Health resources. ChartSpan’s APCM care managers can direct patients to local food pantries, housing and utility agencies, clothing closets, and financial assistance programs.
In addition to providing resources, we can assist QMB patients enrolled in APCM with care goals around exercise, nutrition and other preventative care measures. Our care managers will also check in on patients regularly and follow up when they are released from the hospital or emergency room. Through all these services, we can help QMB patients stay healthier, have lower cost of care, and spend less time in the ER or hospital.
Qualified Medicare Beneficiary Determination: Why It Matters
By learning which of your Medicare patients are QMBs, your practice or health system can avoid billing them accidentally and being forced to issue refunds. Starting in 2025, knowing QMB statuses will also help you identify which patients are eligible for Level 3 of Advanced Primary Care Management.
APCM can provide all Medicare patients with extensive preventative care and your practice with reimbursements. However, these preventative care offerings are especially powerful for QMB patients with two or more chronic conditions.
If you don’t have the time or staff to seek out QMB statuses for your patients, third-party organizations, like ChartSpan, can help. If you partner with us for Advanced Primary Care Management, we will use our approved HETS access to find out which of your patients are Qualified Medicare Beneficiaries. We will then send the list to you for approval. Once those patients are enrolled, they will receive extensive preventative care support while your practice benefits from high reimbursements.
Want to learn more about Advanced Primary Care Management and how it can benefit QMBs at your practice? Check out our guide to APCM, which describes all the features of this preventative care program.
Subscribe for More Insights
Get valuable resources delivered straight to your inbox.
"*" indicates required fields